Ventricular Action Potential
It seems that cardiac action potential is a difficult subject to comprehend for some paramedic students during their cardiac block. When studying cardiology, we need to focus on four components: automaticity, excitability, conductivity, and contractility. For proper function, all must work accordingly and in sync. However, many factors could change the efficiency of these components. Ionic imbalances and damage to cardiac cells could alter cellular activity including action potential.
Before we jump directly into Ventricular Cardiac Action Potential, let’s review some basics of cardiology. Depolarization is the stimulation of cardiac muscle fibers via electrical impulse, leading to muscular contraction. We can also think of it as going from negative charge to a positive charge. Repolarization is the restoration of resting membrane potential (aka relaxation, or recovery of depolarization). We can also think of it as going from positive charge to a negative charge. Ionic balances are crucial to proper depolarization and repolarization. The electrolytes used within this process include sodium, potassium, calcium, and magnesium. Significant changes with these electrolytes will alter cardiac function.
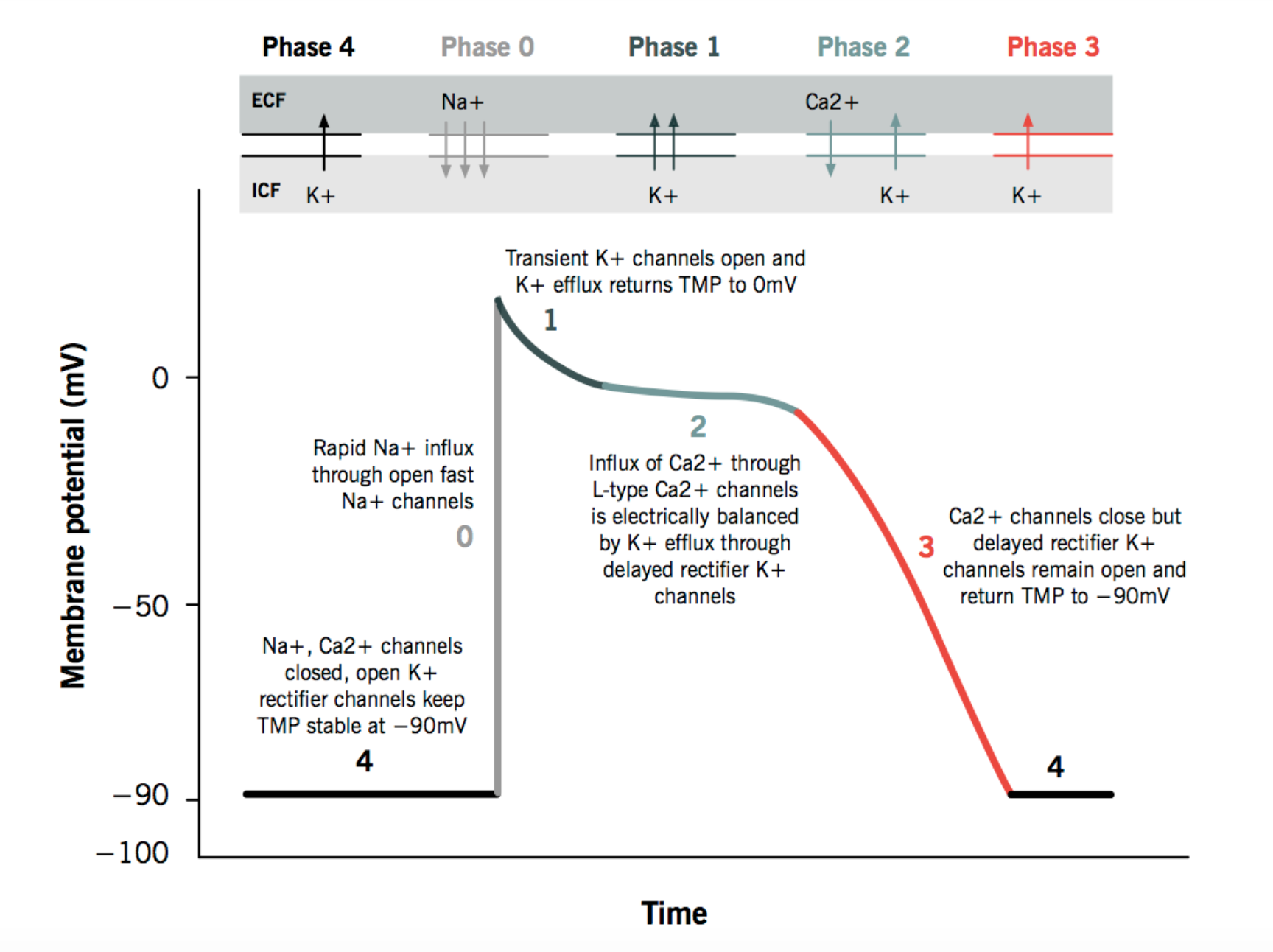
So what is cardiac action potential? Cardiac action potential is the electrical activity (within the cell membrane) during the exchange of electrolytes during muscular contraction. This is measured in milliVolts (mV) as seen on an ekg. Remember, cells at rest have a negative net charge of -90 mV which is relative to the outside of the cell. For action potential to occur, cells must lose that negative charge. An electrical gradient is created across the cell membrane, maintained by chemical pumps in the cell. Just as insulin opens the door for glucose to get into cells, we can think of electrolytes coming through the cellular membrane via doors, or channels. Although electrolytes don’t need doormen, like glucose needs insulin to open the door for them, they do need the doors (or channels) to open. How does this normally happen?
Photo from https://www.researchgate.net/figure/The-sodium-potassium-exchange-pump-mechanism-The-Na-K-pump-that-moves-two-potassium-ions_fig1_221865926
When a myocyte receives an electrical impulse, this stimulates the cell wall to become more permeable. Unlike glucose needing insulin to escort them across the cell membrane, sodium (Na+) doesn’t require the escort and rushes into the cell. The cell now becomes more positive. This is the beginning of phase 0 of ventricular action potential. This is represented by the QRS complex on an ekg.
Photo from https://doctorlib.info/physiology/physiology/16.html
At the same time, calcium (Ca2+) slowly enters the cell through a different door (channel) due to an osmotic gradient (high —> low). As we know, calcium is an important factor in muscular contraction. This causes cellular depolarization, beginning at one point in the cell, moving across like a wave.
Now, if a cardiac myocyte stays depolarized, it can never contract again. It needs to repolarize first. In other words, in order for cells to contract again, they must relax first. Thus we move into the next phase, phase 1, when sodium channels start to close and potassium (K+) exits the cell via briefly opened potassium channels. Potassium is already in the cell because cardiac action potential actually begins at phase 4 where there is intracellular potassium present. In phase 1, Chloride ions that are negatively charged also enter the cell. With fewer potassium in the cell, there are less potassium currents. This leads to less of a plateau at a higher voltage. This is why phase 1 is also called “the notch”.
Photo from http://www.pathophys.org/physiology-of-cardiac-conduction-and-contractility/
After the notch, we move into the plateau phase, or phase 2, which is the longest phase of the ventricular cardiac action potential. It is important to note that there is no plateau phase in atrial cardiac action potential. Sodium and Calcium slowly enter the cell while potassium continues to leave the cell. This is due to delayed rectified potassium channels allowing potassium to leave the cell while calcium channels allow calcium back into the cell (from the sarcoplasmic reticulum). Calcium activates chloride channels to allow Cl- to enter the cell. The movement of calcium and chloride oppose the voltage caused by potassium. The presence of calcium prolongs depolarization. At the end, sodium and calcium slowly enter the cell and potassium leaves, in which the cell begins to repolarize. This phase correlates to the ST segment on an ekg.
Photo from https://step1.medbullets.com/cardiovascular/108015/myocardial-action-potential
Once repolarization begins, we enter the final phase, phase 3. In this phase, calcium channels close, calcium is transported out of the cell. Potassium channels open and there is a rapid movement of potassium out of the cell causing the membrane potential to be negative. At the end, repolarization is complete. The membrane potential is restored to resting value and can now respond to a new stimulus. This phase correlates to the T wave on an ekg.
The resting phase, phase 4, is the return to the resting membrane potential of -90 mV. At this point, the cardiac cycle begins again, waiting for an impulse to be generated.
Phase 4: resting in diastole, waiting for impulse to be generated, K+ inside the cell
Phase 0: impulse received, rapid influx of Na+, slow influx of Ca2+, depolarization and contraction begins, QRS complex on ekg
Phase 1: Na+ channels close, K+ exits the cell, Cl- enters the cell, depolarization ends, partial repolarization begins
Phase 2: Na+ and Ca2+ slowly enter, K+ continues to leave, muscle actively contracting, represented as ST segment on ekg
Phase 3: Ca2+ channels close, Ca2+ transported out of the cell, K+ channels open with rapid movement out of the cell, Membrane potential becomes negative, represented as T wave on ekg, phase 3 ends when Sodium-Potassium ATP pump restores and resting membrane potential is present
Photo from https://www.drawittoknowit.com/course/physiology/glossary/physiological-process/cardiac-muscle-action-potential
Resources
https://teachmephysiology.com/cardiovascular-system/cardiac-muscle/action-potential-ventricular-cells/
https://www.youtube.com/watch?v=rIVCuC-Etc0
Nancy Caroline’s Emergency Care in the Streets, Eighth Edition
Emergency Pathophysiology, Samuel Galvango